Self-vascularizing pseudo-islets for subcutaneous transplantation
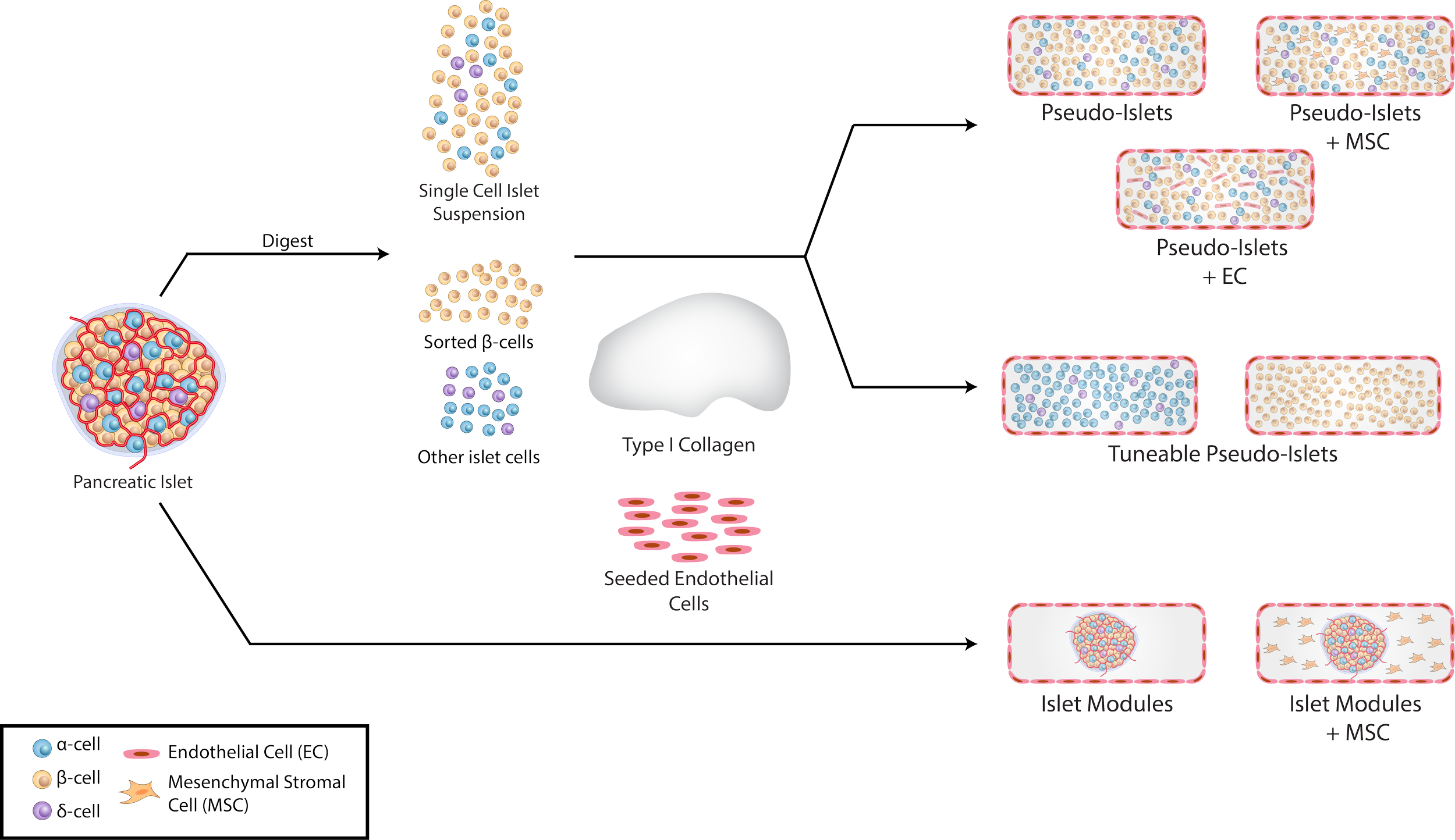
Fabrication of tuneable pseudo-islets. Isolated pancreatic islets were digested into a single-cell suspension and then mixed with type I collagen. After being cut into sub-millimetre rods, pseudo-islets were seeded with Human umbilical vein endothelial cells (HUVEC) on the exterior. Pseudo-islets were fabricated with i) additional cells such as HUVEC or adipose-derived mesenchymal stromal cells (adMSC), ii) different mixtures of α and β-cells.
Following transplantation, islets will experience a state of hypoxia and poor nutrient diffusion before revascularization, which is detrimental to islet survival and affected by islet size and health.
In this study, we engineered tuneable size-controlled pseudo-islets created by dispersing de-aggregated islets in an endothelialized collagen scaffold.
Subcutaneously transplanted pseudo-islets were sufficient in returning streptozotocin-induced diabetic animals to normoglycemia
Whole-implant imaging after tissue clearing demonstrated pseudo-islets regenerated their vascular architecture and insulin-secreting β-cells were within 5 μm of a perfusable vessel – a feature unique to this approach.
By tuning cell composition and the intrinsic scaffold properties, this pseudo-islet platform can allow for a “bottom-up” approach to design a more therapeutic islet construct that can survive engraftment in the subcutaneous space.
3D vascular properties of pseudo-islets at day 21. CLARITY-processed grafts of pseudo-islets at day 21 stained with DAPI (blue, nuclei), GSL-1 lectin (green, vessels) and insulin (red). Insulin+ cells and blood vessels were segmented to create a binary image. Insets (i) highlight a higher magnification volume of insulin+ cells integrating with the perfusable vasculature. The average distance of insulin+ cells in both groups was within 5 μm of a perfusable vessel.
Read our 2021 publication in Biomaterials for more details.